Best practices for Respirator Face Fit Testing in a “post-COVID” world
Respiratory Protection Equipment, or RPE, has undergone rapid evolution and mass adoption during the recent global pandemic.
RPE is a purpose-built subset of Personal Protective Equipment (PPE) and it is used to protect the individual wearer against injury and illness caused by hazardous substances of all types – for example, chemical, biological, and radiological materials typically found in the workplace environment.
As the SARS CoV-2 virus started circulating around the globe killing thousands of people each week, the world began to notice. It became clear there was there a global shortage of tight-fitting respirators, but also a great deal of confusion as to the types of RPE available and their effectiveness and ability to help stop transmission of COVID. It’s reasonable to say that COVID has dramatically changed society’s awareness of and relationship with RPE and elevated the importance of testing its performance characteristics both at time of manufacture and in day-to-day use.
Long before COVID, the role of tight-fitting respirators in preventing or minimizing human exposure to chemical, biological, radiological and a myriad of other toxic substances is well understood and accepted by Industrial Hygienists, Safety professionals and Regulatory bodies around the world.
Since COVID, many new RPE products have been added to what was already a vast array of available choices. Let’s examine the various forms and composition of respiratory hazards to better understand why there are so many different types and classes of RPE on the market today.

Respiratory hazards exist in the form of vapours, fumes and aerosols, the latter containing particles surrounded by other molecules. The sizes of particles that can cause respiratory distress and illness range in size, or ‘fractions’ and are classified as Inhalable, Thoracic, and Respirable. In the OH&S world, these have been defined as particles so large (>10 microns [µ], or “Inhalable”) that they will be deposited on the mucous membranes of the nose and the mouth and thus do not enter the body beyond the larynx, Thoracic, (<10µ, >4µ) which are deposited in the ‘Upper respiratory tract’, and finally, Respirable (<4µ) which can penetrate all the way to the alveoli, those tiny structures in which the lung exchanges carbon dioxide molecules for oxygen. It is here that the most harmful damage and injury to the lungs will occur, such as Silicosis and Pneumoconiosis.
Respirable dust causes damage to the Alveoli and scarring that permanently decreases lung function and can trigger cancer (The EU has recently classified Respirable Silica as a Carcinogen) There is research data published by US CDC/NIOSH showing that extremely fine particles – including nanoparticles and viruses – can pass through the alveoli intact, thus allowing these hazardous agents to pass directly into the circulatory system or ‘bloodstream’ of the exposed worker.
Therefore it has become more important than ever to understand the proper selection, fitting, use and maintenance of RPE for all persons exposed to hazards whether that is in their normal course of work or in the ambient environment (in the case of highly transmissible biological and chemical hazards whether they are naturally occurring or man-made).
It should be noted that RPE is only to be used when adequate control of exposure cannot be achieved by other means, in other words, as a last resort within the hierarchy of control measures: Elimination, Substitution, Engineering Controls, Administrative Controls, and lastly, PPE/RPE. However, in day to day life, RPE has become the ‘first line of defence’ against all airborne hazards including infectious diseases.
Remember, even the highest performing respirators will be of no protective value if the face seal is broached to any significant degree.
Performance of readily available classes and forms of RPE can vary a great deal, based on the demands of the application (e.g. an N95 versus an FFP3,2 or 1, versus a half- or full-facepiece elastomeric respirator) and pre-COVID this was generally consistent with labels showing recognized performance certifications and approvals – based on 3rd party certification testing to established standards such as that performed by CDC/NIOSH at the National Personal Protection Technology Laboratory (NPPTL). However, that is always based on the premise that the respirators do not ‘leak’ at the seal, as fitted to each individual’s face during actual use.

That held true until counterfeit RPE started showing up. Unscrupulous suppliers began producing so-called respirators that appeared to be compliant and were even labeled as such, when in fact they were not capable of protecting the wearer from airborne transmission of the SARS CoV-2 virus or other hazards.
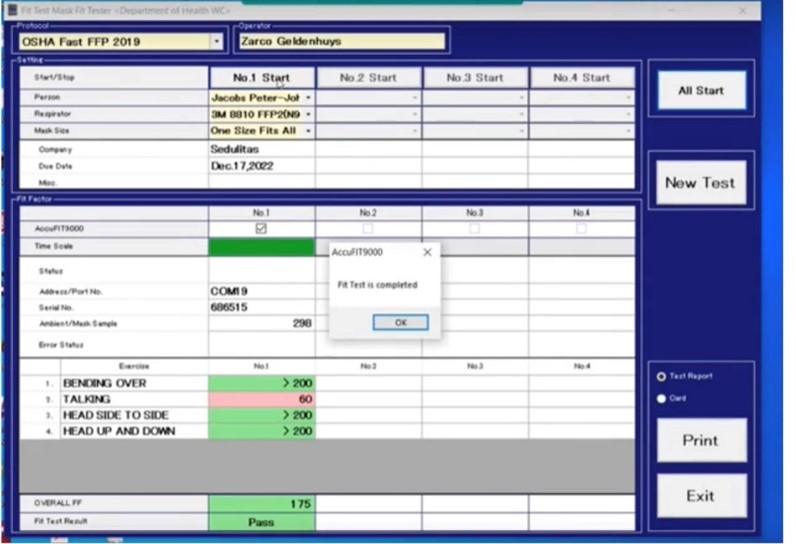
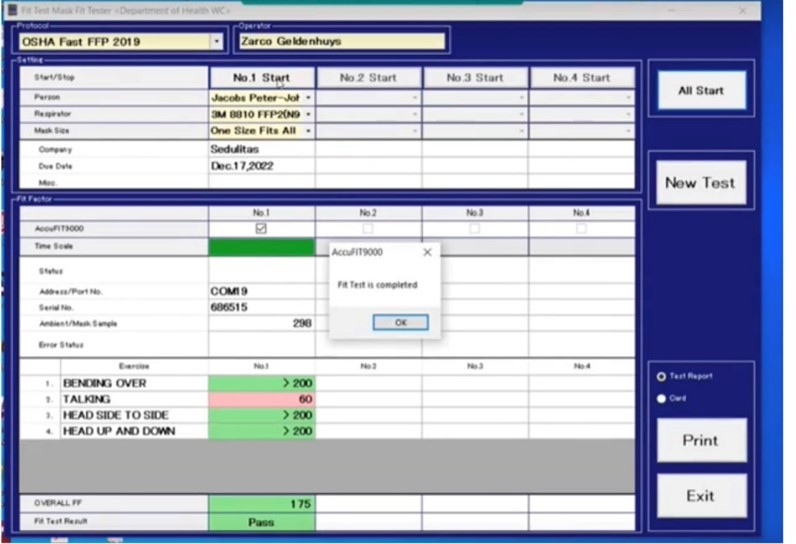
The most effective way of determining whether a supposed piece of ‘compliant’ RPE is actually protecting the wearer is by performing Quantitative Face Fit Testing, which in the case of an FFP or N95 series respirator scientifically determines that the filtration media is in fact truly effective.
Many of the things learned about respirator performance during the pandemic applied directly to the area of respirator fit testing – for a number of critical reasons – perhaps most of all, the urgent need to protect large numbers of first responders, caregivers and others who previously may not have been issued RPE for their daily work routines.
Respirator Fit testing per OSHA CFR 1910.134 has been a mandatory part of all compliant Respiratory Protection Programs (RPPs) in the US. Both Qualitative and Quantitative methods are allowed by OSHA, and Quantitative methods can use either the CNC (Condensation Nuclei Counting) technique, or the CNP (Constant Negative Pressure) technique.
Qualitative methods, using a sweet or bitter challenge agent such as Saccharin or Bitrex® always rely on the test subject’s sensory response – such that if these aerosolized materials are infiltrating a poorly fitting or poorly performing respirator, the subject will sense it and alert the test administrator – resulting in a failed fit test. Quantitative methods rely on an instrument that is purpose-built for performing a measurement to objectively determine if the ‘Fit Factor’ meets the requirements for the class of respirator being tested.
Qualitative fit testing has been used extensively in part due to the perceived cost of acquiring and operating a Quantitative Fit Test device, despite the fact that studies indicate that when administered correctly per the OSHA Protocol, there is a significant human cost in terms of both time spent for each test as well as the risk of RMI (repetitive motion injury) to the administrator, who may be required to squeeze a manual nebulizer thousands of times per day. Add in the amount of work needed to decontaminate a Qualitative Fit test hood, and you have a lot of manual work that interferes with getting a good result in a reasonable amount of time.
When COVID started to hit the workforce in large numbers, however, it became apparent that one of the ‘early onset’ symptoms, Anosmia/Hyposmia and Ageusia/Hypogeusia (full or partial loss of the sense of smell and taste, respectively) could hinder the subject’s ability to accurately respond to the challenge agent(s). Adding in that these symptoms typically occur very early in the infection cycle, where the subjects would still register as ‘negative’ in a COVID Antigen or PCR test, and you can see why there was concern regarding the use of subjective response as a valid indicator of sufficient fit. A session related to this topic was presented by the author of this article at AIHce 2021 (held virtually) titled “Implications of Anosmia and Hyposmia on the Accuracy of Qualitative Respirator Fit Testing”. Further research needs to be done, but by removing the subjective response and using a measuring instrument to determine the fit factor would seem to be more in line with accepted exposure sampling methods used by Occupational Hygienists for decades. Think about that – when was the last time you asked a worker ‘was the noise you heard above 85 dB(A)?’ instead of using a dosimeter or sound level meter to objectively measure their environment?
Qualitative fit testing was not the only method that saw an impact from COVID on the fit test process, however.
Another outcome of COVID was the intense focus put onto air handling / HVAC systems with greatly increased installation of HEPA filtration to try to stop the airborne dispersion of the virus indoors. Vastly reducing the number of respirable particles in the building can have an impact on the operation of Quantitative Fit Test devices using the CNC method as these devices utilize the ambient concentration of respirable particulates in the air as the challenge agent to both the seal and filtration media (in the case of N95, FFP3 and other disposable tight-fitting respirators). Fortunately, this issue can easily be overcome with the newest CNC technology by using a particle generator to supply sufficient levels or aerosol matter. CNP devices are unaffected by this, but the CNP method is incapable of testing ANY N95, FFP Series or KN95 respirators as those respirators cannot form an ‘airtight’ seal – by design.
AccuTec-IHS has taken this technique to another level of functionality through innovation by incorporating a real-time wireless Particle Generator Control function that allows the AccuFIT9000 to turn the free-standing particle generator device on if ambient levels fall below a user-selected level (typically 2-3000 particles/cc) and to turn it back off If levels get excessive (> 6-8000 particles)
Other new innovations in AccuTec’s Fit Test devices is the possibility to power them from a rechargeable external power source, such that fit testing can be conducted at remote sites or anywhere AC mains power is unavailable or intermittent, which is not uncommon in many parts of the world. AccuTec-IHS once again responded to customers’ needs by creating the AccuPACK™ auxiliary power supply to power the RFT device for a minimum of 8 hours and as much as 12 hours.
To be sure, the long-running debate about whether Quantitative fit testing is preferable to Qualitative testing will not go away just because of COVID – but an interesting development that was already underway in other parts of the world could have extreme relevance to how we in the US and elsewhere approach the entire Fit Test process and procedure. And that has to do with certification of the test administrator.
As early as 2014, it was announced in the UK that a Fit Test Accreditation body, called Fit2Fit was formed with the mission of certifying that all persons performing fit tests had been through a comprehensive training program to ensure quality and consistency of the procedure, whether it be Qualitative or Quantitative. This is no different than obtaining CAOHC certification for those who are administering Hearing Tests to prove that they comply with the requirements for producing OSHA required Audiograms for workers who are included in a Hearing Conservation Program
It seems somewhat incongruous to this author that this requirement must be in place for hearing tests but not respirator fit tests, since although hearing loss is devastating to the afflicted worker, and is a compensable injury under OSHA, it does not result in death or terminal illness as certainly can be the case with a worker wearing an incorrectly fitted respirator. And as Quantitative Fit Testing equipment continues to evolve with new capabilities such as wireless control of particle generators to optimize the ambient levels, technicians and test givers need to be aware of their proper use, just as would a certified hearing test provider. Others around the world appear to agree, as countries like Australia and New Zealand are joining the growing list of places where similar accreditations have been issued or being considered.

All in all, the challenges Respiratory Protection Program managers faced when dealing with proper fitting and use of RPE during a pandemic cast a more intense light on the methods, machines and manpower needed to protect workers from all forms of respiratory hazards. Suppliers of fit test products and instruments will continue to innovate, and expectations will grow regarding the certification of practitioners and administrators.
Together, the OHS community and other stakeholders will all play pivotal roles in assuring that the next global pandemic or other unexpected events will be met with even stronger understanding and application of the science, technology and methods needed to do the job right.